Here’s a sneak peek at the first chapter of Dr. Rawls’ new book, Unlocking Lyme, on Lyme disease. Look for upcoming chapters over the next several weeks. Chapter 1 begins with a look at the stealth microbe responsible for Lyme disease…
by Dr. Bill Rawls
Last updated 10/24/16
A Brief History of Lyme Disease
Lyme disease is called Lyme disease because in November of 1975, 51 people (39 children and 12 adults) came down with a mysterious illness in Lyme, Connecticut.1
The event became newsworthy because a cluster of people, all bitten by ticks, suddenly became ill simultaneously. Interestingly, it was a time when people were moving out of cities and into the suburbs to build in tick-filled wooded countryside.
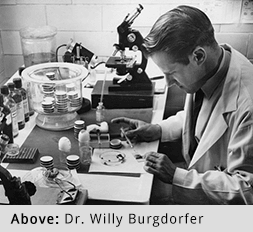
The illness, typified by arthritis and an unusual rash around the tick bite, was first thought to be viral. By 1981, however, a researcher named Dr. Willy Burgdorfer and his colleagues had isolated the now well known corkscrew-like bacteria (called a spirochete) from the blood of victims.
The microbe2 was named in his honor, Borrelia burgdorferi, and the illness was named for the place of origin.
Once people became aware of the new microbe and the illness it caused, cases started popping up all over New England and beyond. Lyme disease seemed to be the newest plague.
An Enigma to Medical Science
From the very beginning, however, Borrelia burgdorferi frustrated both doctors and scientists. Medical science during that era was focused on snuffing out all the horrible poxes and plagues that threatened the lives of every person on the planet. Great progress was being made with new vaccines and synthetic antibiotics and optimism was high that someday all threatening infectious diseases would be eradicated from the planet.
Borrelia hindered that optimism.
Borrelia simply didn’t behave like other microbes and other illnesses that medical science was used to dealing with. It made people sick, but not deathly sick. And some people exposed to it didn’t get sick at all.
The microbe was hard to grow in the lab and extremely difficult to isolate from the blood of people who displayed symptoms (making a definitive diagnosis a real challenge, even today). Though the bacteria was sensitive to most antibiotics in the lab, people often ended up chronically and miserably ill despite antibiotic therapy.
Today, Borrelia burgdorferi and Lyme disease are as much of a mystery as ever before. Public awareness about Lyme disease is at an all-time high, but concern from the medical community is at an all-time low. If something is difficult to diagnose, difficult to treat, difficult to understand, and rarely causes life-threatening illness, doctors simply don’t have time in their busy practices to deal with it.
At the heart of this dilemma is a fundamental lack of understanding of the true nature of Borrelia burgdorferi (and microbes in general).
Lyme Disease, A Prehistoric Illness?
When Lyme disease first debuted, medical science was just beginning to connect the dots between specific microbes and specific illnesses. Doing so was relatively easy with terrible illnesses that had well-defined symptoms, but Lyme disease was anything but well-defined. It took a cluster of similar cases for science (and the media) to take notice at all.
At the time, Lyme disease was labeled as a brand-new illness. It was assumed that new infections with Borrelia spread outward from the point of origin in Lyme, Connecticut. Information that has accumulated in the years following, however, strongly suggests that Borrelia is anything but new.
Even Dr. Burgdorfer and his colleagues suspected they were not dealing with a brand new illness. Physicians in Europe and North America had been describing a tick-borne illness associated with a bull’s eye rash (then called erythema migrans, for the rash emanating from the tick bite3) for hundreds of years. Because the illness typically resolved without treatment, it had received little notoriety.
As it turns out, Borrelia is even much older than hundreds of years…Borrelia is truly ancient.
Borrelia species have actually been found inside ticks trapped in amber dating back 15-20 million years4 (and it may be even older). Over that time period, Borrelia has developed host-microbe relationships with a huge variety of creatures. In fact, this extremely adaptable microbe can infect most anything with blood. Today, the microbe commonly infects mammals, birds, and even some reptiles.
Because ticks have been biting humans since there were humans, it would be logical to assume that humans have been on Borrelia’s list of hosts for a very long time as well. Recently, this fact was conclusively confirmed by a bit of evidence found frozen in a glacier for over 5,000 years.
In 1993, the remains of an ancient human were recovered from in a glacier in the Italian Alps. Remarkably well preserved, the 5,300-year-old mummy yielded a wealth of information to forensic scientists and anthropologists. Findings at a formal autopsy in 2011 revealed a surprise: the genetic signature of Borrelia burgdorferi.
At the time of his death, the mummy was in his mid-forties, showed signs of arthritis and degenerative disease, but was murdered with an arrow in the back. He did not die of Lyme disease.5
This is the most intriguing part about the discovery – the 5,300-year-old man wasn’t severely debilitated. He harbored the microbe6, but was still mobile and functional. At the time of his murder, the man was actually traversing treacherous high mountain terrain in the European Alps (he apparently carried sacks of goods from one community to another).
This is a fundamental point for understanding Borrelia and tick-borne microbes in general. Disabling the host is not Borrelia’s mission. In fact, a bedridden host works against the microbe’s primary purpose.
To complete its life cycle, Borrelia must infect a new host via a tick-bite, reproduce within that host (which only requires maintaining a simple presence of the microbe in the host’s tissues, not an overwhelming infection), and then reboard a new tick when the host is bitten again. That last step, reboarding a new tick, is crucial. If the host is never bitten by another tick, the microbe reaches a dead end. It can’t spread to new hosts.
In other words, the microbe needs a mobile host to fulfill its purpose. The more ticks that bite the host, the better it is for the microbe.
A severely debilitated host is the sign of an imbalanced host-microbe relationship. It suggests that the host’s immune system has been unnaturally compromised.
Borrelia, A Newly Emerging Microbe?
Borrelia is often compared to HIV as a “newly emerging microbe.” Newly emerging implies that such microbial infection is new to the scene and rapidly expanding.
Human immunodeficiency virus (HIV), the cause of acquired immune deficiency syndrome (AIDS), fits the definition of “newly emerging” perfectly. HIV first crossed over into human populations from monkeys in the early mid-twentieth century. It was first recognized in the United States in 1981. Over a very short period of time, HIV rapidly spread across the entire globe.
Most people infected with HIV become severely ill and often die (before drug therapies, most died). Symptoms of HIV are recognizable; it’s easy to tell who’s sick and who isn’t. Because the virus causes overwhelming infection in the host, testing for HIV is very reliable. The incidence of infection within any population of people has always been easy to define.
Infection with Borrelia is the exact opposite. We now know that Borrelia isn’t at all new to humans, and that it has been infecting humans for many thousands of years. Symptoms related to infection are highly variable, and many people infected with Borrelia never get sick. People carrying the microbe without having symptoms are unlikely to be tested.
Testing wasn’t done before 1981, so we have no idea how common it was for people to be infected previously. Testing that has been done over the past 40 years has generally been poor and sporadically performed, certainly not enough to establish a reliable estimate of the true rate of infection.
Though more Borrelia diagnoses are made every year (especially within the past five to ten years), it’s likely a function of better testing (though testing is still far from being ideal), and the fact that more people with symptoms are being tested. Increased awareness artificially skews the data toward appearing that the rate of infection has increased, though it may or may not have.
No doubt, tick populations are being affected by environmental changes, global warming, loss of large animal species, and mobility of human populations, but how this affects the rate of Borrelia infection in humans is truly unknown.
Maybe there are more ticks, but are people actually getting bitten more often? A hundred years ago before industrialization, most people spent most of their lives working outside in fields and woodlands. Tick bites were an everyday fact of life. Today, most people spend most of their time indoors.
Now that researchers are finally getting around to looking for Borrelia in tick populations, they are finding the microbe is quite prevalent. Borrelia has been found in tick populations from the arctic to the tropics7; it’s present wherever there are ticks. Because the relationship between Borrelia and ticks is so ancient, it can be assumed that Borrelia has been present in tick populations worldwide for a very long time.
All of this leaves a very cloudy picture for Borrelia. At this moment, no institution or individual in the world has any idea of how many people are infected with Borrelia, past or present (no matter what they might say).
Without knowing how many people are presently infected with Borrelia or have been in the past, it is absolutely impossible to classify Borrelia as a newly emerging microbe.
An overriding question, one that’s more important than knowing the actual rate of Borrelia infection, is: Are people getting sicker from Borrelia today than they did in the past?
If the iceman of the Italian Alps provides any sort of example, Borrelia wasn’t making people horribly ill 5,000 years ago.
And before 1975, Borrelia wasn’t making people sick enough to even get noticed.
Today, however, almost everyone knows someone who has been touched by the chronic debilitating side of Lyme disease. It’s in the headlines almost every day.
It does appear that the illness of Lyme disease is becoming much more prevalent (or at least more noticed), despite the fact that the rate of infection with Borrelia within human populations may well not have changed much through history.
This is potential cause for concern. The fact that an ancient bacteria that has been infecting humans for many thousands of years is now causing widespread debilitating illness suggests a possible disruption in the balance of nature. It implies that something in the modern world has changed.
This concern, and how it affects our relationship with microbes like Borrelia burgdorferi, will be thoroughly explored in upcoming chapters. It’s the key to understanding Lyme disease and most chronic illnesses that have become so prevalent during our modern times.
Key Takeaways:
- Borrelia is spread primarily by ticks, but also by other biting insects.
- Borrelia can adapt to a huge variety of natural hosts.
- Borrelia has been infecting humans for a very long time.
- Borrelia burgdorferi is widely distributed in ticks worldwide and commonly infects humans.
- Because of environmental disruption and mobility of people, tick-borne diseases may be changing, but whether this translates into an increase in human infection rate is unknown.
- Because infection with Borrelia is hard to diagnose and difficult to define, no organization has any idea how many people worldwide are infected.
Dr. Rawls is a physician who overcame Lyme disease through natural herbal therapy. You can learn more about Lyme disease in Dr. Rawls’ new best selling book, Unlocking Lyme.
You can also learn about Dr. Rawls’ personal journey in overcoming Lyme disease and fibromyalgia in his popular blog post, My Chronic Lyme Journey.