Dr. Rawls Explains Why Virulence Matters
by Dr. Bill Rawls
Last Updated 10/31/16
Here’s the fourth installment of Dr. Rawls’ new book, Unlocking Lyme on Lyme disease. This chapter focuses on the differences between high virulence and low virulence as it applies to microbes.
All the microbes described so far have one thing in common — they are host dependent.
And host dependency is at the root of most problems caused by microbes.
Host dependent microbes must, by necessity, scavenge resources and essential raw materials from the host’s body. Though harm is unintentional, a certain amount of harm is done by the process of extracting resources from a less-than-willing host. Illness occurs when harm is significant or accumulates.
Virulence is the potential for a microbe to cause harm or illness. All host-microbe relationships are defined by virulence.
Throughout life, you are continually exposed to microbes seeking new host relationships. It is what microbes do. Spreading from one host to another is their purpose in life. Because environments are constantly fluctuating, adapting to new hosts helps ensure survival of that microbe’s species. The most successful microbes, like Borrelia, quickly adapt to new environments and have adapted to a wide range of hosts.
An infection from a microbe is simply a microbe attempting to use you as a host.
Each and every time you have ever gotten bitten by a tick, mosquito, flea, or some other biting insect, been nipped or scratched by a dog or cat, scraped or cut your skin, had sex with another person, kissed another person, even hugged another person, picked your nose, put your fingers in your mouth, given birth, been born, used a public toilet just after someone else had been there, taken a breath just after someone sneezed, been swimming in a natural pond, lake, or river, or consumed any food or beverage… you have encountered host-seeking microbes.
You are exposed to many thousands of different kinds of microbes every day.
Fortunately, your immune system is extraordinarily sophisticated. It evolved as a result of repetitive exposure to an enormous number of different microbes over millions of years. For every new trick that different microbes have come up with to confound immune functions, the immune system has developed countermeasures to match it. Each and every countermeasure is permanently wired into the your immune system.
Therefore, most host-seeking microbes are immediately recognized and either dispatched or suppressed — so much so that most of the time you’re not even aware that a confrontation has occurred. Rare is a confrontation that causes illness and even rarer still, an illness that is truly life-threatening.
In other words, the more familiar your immune system is with a particular microbe, the lower the potential for that microbe to cause you harm (lower virulence). If the immune system knows a microbe (the human immune system has confronted it before), then the natural aggressiveness of that microbe is curbed and harm is minimized. In some cases, the microbe and the host enter a balanced relationship in which the microbe persists and the host is not significantly harmed.
This is the case with microbes referred to as normal flora. Your relationship with these microbes is so well balanced that the microbes gain benefit, but also provide benefit in return — the relationship is symbiotic. This type of mutual adaptation of one species to another requires thousands upon thousands of years of exposure between the host species and the microbe species. Our relationship with our normal flora dates back thousands of years; we are extremely familiar with them.
At the other end of the spectrum, if the host’s immune system has no familiarity with a microbe, then the immune system has no ability to inhibit the natural aggressiveness of the microbe.
This is what happens with an Ebola outbreak. Humans have rarely been exposed to the Ebola virus and the human immune system has no familiarity with it. When a human host is infected with Ebola, the resulting host-microbe relationship is extremely unbalanced (and unnatural). The immune system of the infected person is completely blindsided and the person quickly becomes severely ill. A wake of destruction spreads like wildfire until it eventually burns out.
For humans, Ebola is possibly the most virulent microbe on the planet. On a 1 to 10 scale of virulence, Ebola would be a definite 10 (see Chart 4.1).
Interestingly, microbe virulence is host specific; what is one host’s pathogen is another host’s normal flora. Every host-dependent microbe has a balanced relationship with at least one natural host (and some microbes, like Borrelia, have many natural hosts). For the Ebola virus, the natural host is thought to be a spider that lives in Africa. In that host, it exists without causing harm; the relationship is well balanced. On the spider’s virulence scale, Ebola virus would be only a 1.
Similarly on our virulence scale, our normal flora, the microbes that inhabit our intestinal tract, skin, and airway passages, would also be at 1. The potential for these microbes to cause illness is extremely low (but not zero).
Everything on the human microbe virulence scale falls between 1 and 10. Microbes can be loosely separated into high virulence (5-10) and low virulence (1-5). The general traits and habits of high virulence microbes are very different than those of low virulence microbes.
High virulence microbes are much more apt to cause acute life-threatening illness and require acute medical intervention. Symptom profiles are typically indicative of the specific microbe causing the illness (most doctors would be able to identify AIDS, Ebola, or malaria from the symptoms alone). Chronic infections with high virulence microbes (such as malaria), usually manifest as relapses of acute symptoms.
Chart 4.1 Virulence Scale
Initial infections with lower virulence microbes (<5 on the scale) are typically mild and generally resolve without treatment (the immune system immediately makes recognition and takes countermeasures). Resolution of symptoms, however, does not necessarily mean the microbe is gone. Chronic infections can manifest with vague and nonspecific symptoms (such as those common to Lyme disease). Microbes at the lower end of the virulence scale are less likely to respond to conventional therapies such as antibiotics and vaccines.
Note that the virulence scale can vary from person to person (we are all slightly different). One person’s immune function against a particular microbe may be different from another person’s (genetic memory). It depends on where one’s great ancestors roamed the planet and what types of microbes they were exposed to. People from certain regions of Africa where malaria is endemic are much more resistant to malaria than all other people.
Some people are more apt to get sick from Borrelia than others. The same is true with Mycoplasma, Bartonella, Babesia, or any other microbe.
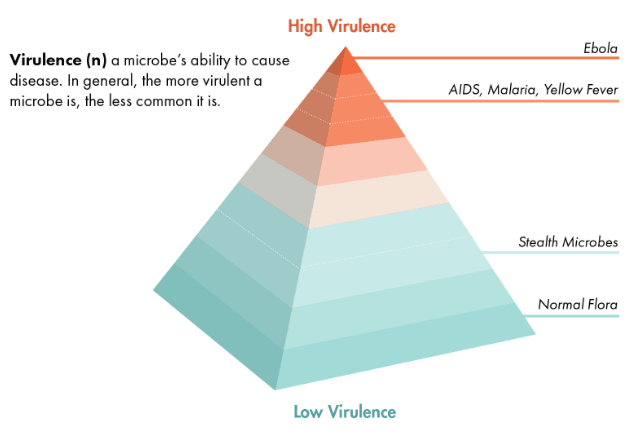
The Virulence Pyramid
An interesting phenomenon that holds true for most microbes is that risk of exposure to a certain microbe is inversely related to its virulence. In other words, the more virulent a microbe is, the less likely you are to encounter it. Most people on the planet will never be exposed to Ebola virus or HIV (even though these microbes notoriously get the most press attention). Everyone on the planet, however, has a balanced relationship with microbes that are considered normal flora.
Risk of exposure can be represented by stretching the virulence scale out into a pyramid shape (see Chart 4.2). Highly virulent pathogens such as Ebola virus and HIV are represented at the very peak of the pyramid; risk of exposure is fortunately extremely low.
The broad base of the pyramid represents our normal flora. Every person on earth harbors benign microbes classified as normal flora; exposure is universal.
Chart 4.2 Virulence Pyramid
As you can see from the pyramid, there are a lot more microbes below the level of 5 than above it. Over many thousands of years, humans have developed familiarity with most microbes that we will likely encounter. Because of host-microbe familiarity, they are less virulent.
This is especially true of tick-borne microbes. Because ticks have been carrying microbes as long as there have been ticks, and ticks have been biting humans as long as there have been humans, humans are well acquainted with most microbes that ticks carry.
The tick-borne microbes most commonly associated with chronic Lyme disease all fall below 5 on the pyramid scale. Mycoplasma, Bartonella, and Chlamydia are found in the 2-4 range. Borrelia is slightly more virulent (more apt to cause illness) and would fall in the 3-5 range.
Ticks can carry higher virulence microbes, but they are rare. Powassan virus is the most virulent of all the tick-borne microbes. It is the only tick-borne microbe that would achieve a 10 on the virulence scale. If you even survived an infection with Powassan virus, it would leave you with permanent neurological damage. As you might predict, it is extremely rare (only 60 cases over the past 10 years). There is no cure, and because it is so rare, there probably never will be.
Rickettsia rickettsiae, the microbe that causes Rocky Mountain Spotted Fever, is next on the list of higher virulence tick-borne microbes with a score of 7-8. As you might expect, infection with R. rickettsiae is much less common than with Borrelia. Ehrlichia and Anaplasma are more common than R. rickettsiae, but also less virulent (4-7 on the scale). Babesia, though it is a protozoa instead of a bacteria, has similar potential to cause illness and would be found at 4-7 on the scale.
These microbes are more apt to cause severe acute disease, and less likely to cause chronic illness. Chronic illness, when it occurs, is generally associated with relapse of acute symptoms.
Interestingly, these microbes have been around just as long as Borrelia and the others, but human exposure may have been different through the course of time. There is some evidence that Borrelia is better at infecting than Rickettsia, so even though both microbes may be prevalent in ticks, human exposure may have been different.
The Microbiome and Stealth Microbes
The total collection of all the microbes in the body is referred to as the microbiome. There are many thousands of different microbe species, totalling 100 trillion microbes, that make up the human microbiome. A person’s microbiome is as unique as his or her genes.
The microbiome consists predominantly of microbes considered to be normal flora, but it also contains microbes that would be considered “marginal.” They are outliers… misfits… and we all have them. We collect them as we go through life. They enter the body at every opportunity by breaks in the skin or bug bites, consuming them in food or drink, breathing them in, or sexual contact.
The human immune system is familiar with these microbes, but not enough to accept them as normal flora. They have higher potential to cause harm than normal flora, but they are still not high virulence (2-5 on the virulence scale). Mycoplasma, Bartonella, Chlamydia, and Borrelia are certainly on the list, but there are many many others; the list would also include viruses, such as Epstein-Barr virus (EBV), Cytomegalovirus, and other herpes-type viruses.
They would like to join the normal mix of microbes in the body, but they haven’t quite learned how to fit in – they are normal flora wannabes. Because of their questionable status, an open invitation is never issued and the immune system makes every effort to oust them.
Persisting is their specialty, however. They are experts at manipulating the immune system to stay one step ahead. It becomes a perpetual tug-of-war that neither party ever wins. The microbes are marginalized and the potential for harm is minimized (their natural aggressiveness in kept in check), but they stubbornly prevail in the margins of the body .
Because of their fugitive status, they act very differently than normal flora. Normal flora typically inhabit the skin, the gut, and other body cavities. Marginal microbes seek out immune privileged sites in the body (brain tissue, joint cartilage, eyes, biofilms, and inside cells), where they are less apt to be targeted by immune functions.
For this reason, they are often called stealth microbes.
They are constantly pursued by the immune system and therefore typically occur in low concentrations in the body and grow very slowly (remember, that’s all they need to do to complete their mission). This makes finding them extraordinarily challenging and getting rid of them even more challenging.
As long as healthy immune function is maintained, stealth microbes remain marginalized and do not cause overt illness.
Let immune function falter for even for an instant, however…
Stealth Microbe Characteristics
- Strategies vary between microbes, but characteristics are similar.
- They are well adapted to human hosts, but not as well adapted to normal flora.
- Initial infection is generally mild; most infections resolve without treatment.
- Severe infection is unusual – they rarely kill people directly.
- Multiple stealth microbes are present in the margins at one time.
- Everyone harbors stealth microbes, but people with chronic illness may harbor a wider spectrum of stealth microbes.
- Because of being constantly suppressed by immune function, they occur in low concentrations in the body and grow very slowly (even when intense symptoms are present).
- They have the ability to live inside cells, protected from immune function.
- Most stealth microbes can infect white blood cells and be spread throughout the body.
- Symptoms, when they occur, are related mostly to the generation of inflammatory cytokines, and less by direct damage by the microbe.
- When symptoms occur, they are mostly systemic (not localized) and mostly nonspecific (fatigue, achiness, migrating joint pain, brain fog, nerve conditions, anxiety, insomnia, depression, intestinal dysfunction).
Dr. Rawls is a physician who overcame Lyme disease through natural herbal therapy. You can learn more about Lyme disease in Dr. Rawls’ new best selling book, Unlocking Lyme.
You can also learn about Dr. Rawls’ personal journey in overcoming Lyme disease and fibromyalgia in his popular blog post, My Chronic Lyme Journey.