by Dr. Bill Rawls
Updated 1/19/21
To truly understand Lyme disease, you must understand the nature of microbes. This article places Lyme disease in perspective with other known microbial diseases by taking a close look at virulence, the level of a microbe’s ability to cause damage or disease in the host.
I’ll explain why Lyme is a chronic infection of not one microbe, but multiple microbes, and why chronic Lyme disease must be treated differently than acute microbial diseases. I’ll also provide evidence for links between Lyme disease and other chronic degenerative diseases such as fibromyalgia, and offer natural solutions that best fit the level of the microbe’s virulence.
Microbes Are Ubiquitous
Microorganisms, aka microbes, are microscopic single-celled living organisms that are invisible to the naked eye. The term “microbe” is very general. It includes mostly bacteria and viruses, but also protozoa and certain types of fungi.
Because microbes are invisible, sometimes we forget how pervasive they really are. In reality, microbes are everywhere; they are able to thrive in every environment on earth. Every living organism is colonized by microbes — including your body.
At this very moment, trillions of microbes are living in and on your body. The sum total of all the microbes that inhabit your body is called the microbiome. It includes somewhere between 20,000 and 40,000 bacterial species, but scientists have just begun to catalog all the viruses. With an infinite number of different combinations, your microbiome is different from every other person’s on the planet.
You’ve probably heard of some microbes being called “good” or “bad,” but they can’t be defined that way — they’re simply trying to survive. The microbes that we encounter are host dependent, which means they must acquire the nutrients necessary for survival from a host like us.
Microbes that inhabit the body are concentrated mostly in the gut and on the skin. Bacteria and other microbes in the gut survive off of the leftovers from food that you don’t absorb. On the skin, they survive off of oils you secrete to lubricate your skin.
Availability of food is the primary factor that affects growth of microbes like bacteria — they keep growing as long as food is present. Not surprisingly, the highest concentration of bacteria and other microbes is in the intestinal tract where there’s plenty of free food. Because nutrients on the skin are sparse, the concentration of microbes is much lower than in the gut.
How Microbes Break Through Your Barriers
The problem with microbes is a matter of resources: The carbohydrates, fats, proteins, vitamins, and minerals that make up the cells of your body are also potentially a source of food. In fact, your cells are such an exceptionally good food source for microbes that the body must maintain barriers to keep the organisms out.
The primary barriers of the body include:
- Skin
- Mucous membranes that line the mouth and nasal passages
- Stomach and intestinal linings
- Bronchial passageways in the lungs
- The skin of body openings, such as the ears and vagina
Microbes are always looking for an opportunity to break through barriers — an infection is just a microbe trying to find a way inside your tissues to get at your cells. If they can make it through and enter the bloodstream, then they have access to all the cells inside the tissues of your body. That’s where microbes cause harm — by consuming cells of the body.
Unfortunately, the barriers of the body aren’t nearly as secure as you might hope. A study in 2015 found that bacteria from the gut constantly trickle across the intestinal barrier into the bloodstream. It happens in everyone, but it’s more pronounced if the balance of microbes in the gut has become disrupted by chronic stress and a steady diet of carb-loaded processed foods.
Any break or cut in the skin also gives microbes on the skin, such as staph or strep, the opportunity to invade deeper tissues and consume the unprotected cells just below the skin surface. A skin infection is simply bacteria consuming cells in tissues below the surface of the skin.
It’s not just the microbes that are already on or in your body that you have to worry about, however. Microbes from the outside environment are constantly trying to break through barriers to get into your body, too — the nutrients and resources that your cells have to offer are just too good to ignore!
Different microbes choose different pathways. Some microbes, such as influenza and coronavirus, ride on air droplets to enter the body by way of the nasal passageways and lungs. All it takes is one infected person in a crowded space to infect the entire room.
Intimate contact is another popular route for microbes to take into the body. The list of microbes that can be transmitted by sexual contact is longer than you might expect.
And then there are blood-sucking insects. Who hasn’t been bitten by a tick, biting fly, mosquito, or flea? The idea that only certain ticks carry the microbes that cause Lyme disease is correct, but every tick carries hundreds of different species of microbes. Blood-sucking insects are nature’s perfect vehicle for spreading microbes. Why wouldn’t lots of different microbes take advantage of such an opportunity?
The only thing that prevents microbes from ravaging the cells of your body is your immune system. When a foreign microbe crosses a barrier or enters the bloodstream, it encounters the defenses of the immune system.
White blood cells (WBCs) of the immune system line every barrier in the body and circulate throughout the bloodstream — a single liter of blood contains somewhere between 4 and 11 billion WBCs. Your immune system is constantly on guard to defend your cells.
The Virulence Factor
The potential of a microbe to break through barriers and ravage cells of the body is called virulence. Virulence is a function of both the natural aggressiveness of the microbe and how familiar the immune system is with a particular microbe. Of the two, the immune system’s familiarity is most significant.
The human immune system is extraordinarily sophisticated. It evolved over millions of years of repetitive exposure to an enormous number of different microbes. For every trick that microbes devised to get past immune system barriers, the immune system developed countermeasures to match it — layer upon layer of different levels of protection are hardwired into your genes for countless numbers of microbial threats.
It means that the more familiar a microbe is to your immune system, the better it can manage it. A pathogen (disease-causing microbe) is just a foreign microbe that your immune system doesn’t know very well and therefore isn’t pre-equipped to handle.
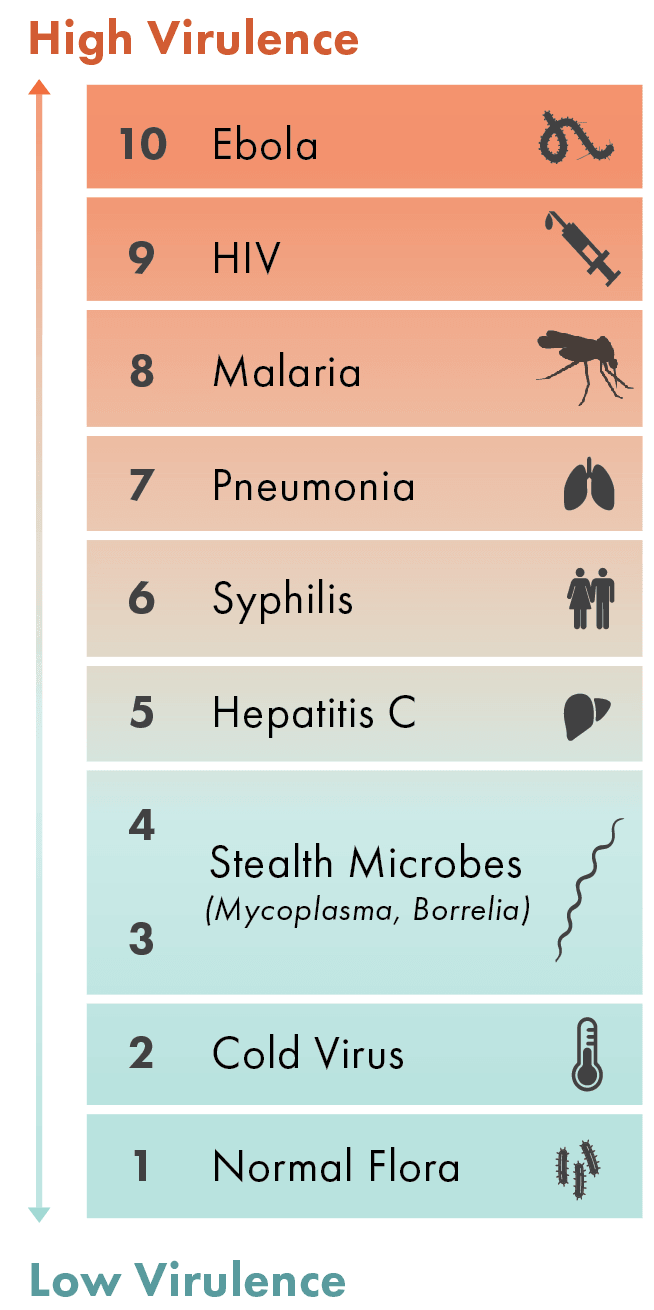
Of course, there are different degrees of pathogens. The higher a microbe’s potential to do harm, the greater its virulence.
Possibly the most virulent microbe of our time is Ebola virus. Most anyone who becomes infected with Ebola virus becomes severely ill, and the mortality rate can be as high as 60%.
The reason that Ebola is so threatening is because humans have rarely been exposed to it, therefore the immune system has no built-in defenses against it. On a scale of 1 to 10, Ebola would be a definite 10. Other than possibly HIV, there’s not much that can match Ebola virus’s potential to ravage cells of the body.
At the opposite end of the spectrum are the microbes that dominate our skin and body cavities (throat, lungs, stomach, intestines, genital openings). Defined as normal flora, these microbes would be 1 on the scale — not zero, because even our normal flora have potential to do harm, but that potential is very low.
Your immune system “knows” the microbes defined as normal flora better than any others — it’s a relationship that’s been honed over millions of years. By being able to keep the natural aggressiveness of these microbes completely in check, a mutually beneficial relationship becomes possible. In trade for the nutrients and resources you provide, they give back by helping to digest food, providing certain vitamins (B12, vitamin K), and preventing overgrowth of more threatening microbes that are always present.
Of course, there are a wide variety of microbes that exist between Ebola (10) and normal flora (1). As a general rule, the more virulent a microbe happens to be, the less common it is, and vice versa. This would be as expected; the more common a microbe is in nature, the greater the chances of the immune system having had repetitive exposure to it.
This works out mostly in our favor: The chances of being exposed to a highly virulent microbe such as Ebola virus are quite rare for most people, but everyone is exposed to cold viruses on a regular basis. Viruses that cause the common cold have been following humans around since the beginning of humans, and therefore, the human immune system is extremely familiar with them. They would come in at about 2 on the virulence scale.
Virulence decreases with exposure. Once someone has been infected with a microbe and recovers, the immune system “learns” to manage that microbe and it becomes less of a threat. Vaccines provide an opportunity for the immune system to learn to deal with a microbe without suffering the consequences of an infection with the actual microbe.
Virulence can also vary from person to person. This has been very evident with the COVID-19 pandemic, where half the population hardly gets sick at all with exposure to the virus, but some people can get extremely sick. It all has to do with whether a person’s immune system has built-in immunity to the virus.
A Strategy of Stealth
Foreign microbes don’t necessarily have to be highly virulent to be successful. In fact, some of the most successful microbes trade virulence for persistence. Often called stealth microbes or stealth pathogens, these sneaky opportunists specialize in staying just under the immune system’s radar. They enter the body with little fanfare or commotion. Initial symptoms may be mild, if they occur at all.
Though the immune system is familiar with them, these microbes are masters at persisting — chronic infections are common. Unlike normal flora that call your body home, their mission is maintaining a presence in tissues of the body and waiting for an opportunity to spread to other hosts. Because of their stealthy nature and because they are remarkably common, these are the microbes you should worry about most.
One key strategy that stealth microbes use to persist inside the body is invading and living inside cells (called intracellular). Infecting and living inside cells of other living organisms is an ancient strategy that microbes have been honing for billions of years.
By infecting and pirating organic molecules and resources from larger cells (the ultimate dine-in experience), microbes can survive without having to work very hard. Living inside another cell offers food and protection, from the immune system, other bacteria, and antibiotics. It’s an easy living strategy used by many bacteria, some protozoa and yeast, and all viruses.
Borrelia burgdorferi, the bacteria commonly associated with Lyme disease, is one such microbe. Borrelia has been infecting humans by way of tick bites as long as there have been humans — the human immune system is very familiar with it. It’s present in various species of ticks worldwide, from the tropics to the arctic circle. On the virulence scale, it would be about a 4 in most people.
After entering the bloodstream by way of a tick bite, Borrelia infects white blood cells and disperses to tissues throughout the body (joints, brain, heart, everywhere else), where it infects and lives inside cells. Though the immune system would like to eradicate this pest completely, Borrelia is so proficient at maintaining a presence that often a stalemate is reached in which the bacteria maintains a low-grade presence in tissues.
Often people don’t even know they’ve been infected. Tick bites frequently go unrecognized, and symptoms at the time of acute infection are often mild, if they occur at all. Once established in tissues, the fact that Borrelia lives inside cells and occurs in low concentrations makes it difficult to diagnose and almost impossible to eradicate with antibiotics.
In a healthy host, the bacteria can stay dormant in tissues for years —even for a lifetime — without causing symptoms. Let the immune system falter for any reason, however, and bacteria can erupt and cause symptomatic illness. Because bacteria are erupting throughout tissues in the body, a wide range of symptoms are possible, including fatigue, brain fog, joint pain, muscle pain, intestinal problems, and feeling flu-ish.
Borrelia is One of Many Stealth Microbes
Borrelia is far from being the only stealth microbe. All of the recognized Lyme coinfections are stealth microbes, but that may be just scratching the surface.
When chronic Lyme disease sufferers are tested for coinfections, most are found to be carrying more than one of several possibilities including mycoplasma, bartonella, babesia, chlamydia, ehrlichia, and anaplasma. Testing, however, is limited to one or a few species of certain bacteria — dozens of species are possible for each bacteria.
Ticks alone carry hundreds of different microbes, but some of these bacteria are more commonly spread by other routes. Mycoplasma pneumoniae and Chlamydia pneumoniae are common respiratory infections that most people pick up as kids. Other species of mycoplasma and chlamydia are commonly spread by intimate contact with other people.
And then there are the viruses. Many people with chronic Lyme disease are also found to have reactivation of Epstein-Barr virus (EBV), cytomegalovirus (CMV), HHV-6 types a and b, HHV-7, HHV-8, and/or parvovirus.
All of these microbes sit within the lower half of the broad base of the virulence chart. Therefore, it shouldn’t be surprising that there are so many possibilities: Microbes that fit the description of stealth microbes are remarkably common. The fact of the matter is that every living organism on earth — plants, mushrooms, animals, and people inclusive — harbor some cells infected with microbes.
Characteristics of Low-Virulence Stealth Microbes
- Initial infection is generally a mild event.
- Asymptomatic chronic infection is common — chronic symptomatic dysfunction only occurs if immune system functions are disrupted.
- Chronic infection is associated with vague, nonspecific symptoms (fatigue, brain fog, tingling in extremities, joint pain, muscle pain) that are unrelated to the initial infection.
- Chronic infection is associated with low concentrations of the microbe in the body, often making diagnosis challenging.
- Stealth microbes have a slow growth rate.
- They are intracellular – microbes have the ability to live inside cells.
- Chronic infection with stealth microbes typically responds poorly to antibiotics and vaccines.
- Symptoms result from inflammation resulting from manipulation of the immune system by the microbes, not as much from direct harm by the microbe.
- They take the path of least resistance and gravitate toward sites of established inflammation in the body (twisted knee, eye abrasion, liver overburdened with toxins).
- Stealth microbes work together; chronic infection with multiple microbes is the norm.
No doubt, infection with multiple stealth microbes at once increases virulence. Each of the above mentioned microbes uses a slightly different strategy for outmaneuvering the immune system. Several stealth microbes together can disrupt immune system functions enough to open the door to chronic symptomatic infection.
In other words, virulence is additive – multiple stealth microbes together may have a higher potential to cause symptomatic illness.
Chronic Lyme disease is rarely (possibly never) a disease caused by one microbe. Multiple stealth microbes come together to cause chronic Lyme disease.
Infection with multiple microbes does not always occur simultaneously, though it can happen with the same insect bite. A stealth microbe such as mycoplasma or bartonella may be present (possibly for a long time) without causing symptoms. Then a tick bite transmitting borrelia or other tick-borne microbes comes along and disrupts immune system functions enough to allow symptomatic illness.
Borrelia doesn’t even have to be involved. Coinfections can occur with any of the above microbes without borrelia. Because stealth microbes cause similar nonspecific symptoms, chronic infections with other stealth microbes can look just like Lyme disease.
This is where the margins start to blur between chronic Lyme disease and other chronic illnesses like fibromyalgia and chronic fatigue syndrome (ME/CFS).
If you draw circles around the symptoms associated with Lyme disease, chronic fatigue, and fibromyalgia, the circles deeply overlap. The nonspecific symptoms commonly associated with any one of the listed stealth microbes sit right in the middle of those overlapping circles.
In other words, the possibility that fibromyalgia and chronic fatigue are also associated with stealth microbes is extremely high. Variations in symptoms depend on the microbes present. The list of known stealth microbes gets longer everyday, and who knows how many are waiting to be discovered.
It’s rarely the microbes alone that cause chronic illness, however. Stealth microbes are remarkably common; avoiding acquiring some of them is nearly impossible. It’s other factors that disrupt immune system functions and tip the balance toward chronic illness.
There Is An Epidemic of Chronic Immune Dysfunction
The steady rise in chronic diseases like Lyme disease, fibromyalgia, chronic fatigue, and autoimmune and other degenerative diseases over the past 75 years is disturbing, but explainable. The underlying problem is not an epidemic of emerging stealth microbes (stealth microbes have been around for thousands of years), but instead something that we have brought on ourselves.
The modern world has become saturated with environmental factors that disrupt immune function, with four in particular doing the bulk of the damage.
The Most Prevalent Immune Disruptors




These modern stress factors come together to cause widespread chronic immune dysfunction in much of the world’s population. This opens the door for chronic infections with stealth microbes that otherwise would not have been such a threat.
Global warming, increased ticks, and people spending more time outdoors may also fit into the equation, but these outward factors matter less than you might think.
Stealth microbes have always been there and they always will be…just waiting for an opportunity!
The Best Solutions are Defined by Virulence
Highly virulent microbes must be addressed with a compatible level of potency. Targeting specific microbes with specific drug therapy (antibiotics, antivirals, vaccines, other supportive drugs) is the best approach for controlling highly virulent microbes. Acute infections such as Rocky Mountain Spotted Fever generally respond well to antibiotic therapy. The Ebola epidemic in Africa has been almost completely controlled with quarantine alone.
The classic “identify, target, and destroy” approach that works for high virulence microbes, however, is not a good fit for stealth microbes. First of all, it’s hard to know what to target. Even if one microbe is revealed by testing, the possibility of many other hidden stealth microbes being present is much too high to ignore.
The very nature of stealth microbes makes them resistant to conventional therapies. Even when stealth microbes come together to cause significant chronic illness, they still retain their individual stealth characteristics. Slow growth, low concentrations of bacteria, and the ability to live inside cells and isolated areas of the body dramatically limit the usefulness of synthetic antibiotics. And the ability of stealth microbes to continually alter genetic signature renders vaccines worthless.
The best solutions are actually not high tech. Normal health can be restored by creating a healing environment within the body. Minimizing immune disruptors by eating a clean diet, eliminating unnecessary toxins, reducing oxidative stress with antioxidants, managing stress, and exercising regularly is essential for becoming well.
Natural herbal therapy is a perfect complement. Many herbs reduce inflammation and enhance immune function, while at the same time suppressing stealth microbes. Because herbal therapy is so remarkably safe, it can be continued for a lifetime.
1. Begin with Herbal Therapy.
If you’re looking for a practical means to bolster your immune system and protect the health of your cells, I recommend starting with plants. Like humans, plants must protect themselves from a wide range of stress factors: damaging free radicals, physical stress from harsh weather, toxic substances, harmful radiation, insects, invasive fungi, parasites, and, last but not least, every variety of microbe.
The chemical substances that plants use to combat threats and safeguard themselves are called phytochemicals. Phytochemicals are made up of a diverse assortment of hundreds of different chemical compounds that serve a variety of needs via numerous mechanisms. Some are antioxidants that protect cells from different types of free radicals, toxic substances, and harmful radiation. Others promote the balance of communication systems within the plant and contain a myriad of antimicrobial phytochemicals.
The herbs that top my list (and that are most widely available) for anyone dealing with Lyme disease and stealth microbes include:
You don’t have to take all of these herbs to experience benefits, but taking more than one herb at a time broadens the range of coverage against the stealth microbes that may be present.
2. Stock Up On Micronutrients for Your Cells.
Your cells use up a lot of essential nutrients that are necessary for optimal function when you’re stressed or dealing with a chronic illness like Lyme disease. To counteract this, I recommend complementing herbs with a combination of supportive, natural micronutrients:
Glutathione
This essential antioxidant plays a key role in protecting mitochondria (the powerhouses of cells) from free-radical damage, as well as enhancing detoxification processes and fortifying immune functions. To maintain your glutathione reserves, supplement with 500-1,000 mg reduced powdered glutathione twice daily (doses are dependent on preparations used).
N-acetyl cysteine (NAC)
A precursor to glutathione with antioxidant and anti-inflammatory properties, NAC helps to protect cells from damage and oxidative stress. To optimize NAC levels, supplement with 500 mg twice daily. (Note that doses are dependent on preparations used.)
Vitamin D
Known as “the sunshine vitamin,” vitamin D is critical for normal immune function. Vitamin D is created in the skin with exposure to UV rays of sunlight. Because most people have low sun exposure (or use sunscreen, which blocks vitamin D production), low vitamin D levels are common. A simple blood test from your healthcare provider will tell you if your levels are adequate (> 40ng/ml).
Vitamin D3 is the preferred form of supplementation. Depending on the starting level, you may benefit from anywhere between 1,000 and 4,000 IU daily.
Vitamin C
Another key player in healthy immune function, vitamin C has known antiviral, anti-inflammatory, antioxidant, and immunomodulating properties. With chronic infections, our stores of vitamin C can become depleted. The body needs extra vitamin C when under stress, so aim for 500-1,000 mg of buffered vitamin C daily.
3. Nourish Your Body.
Beyond herbs and micronutrients, another key to preventing the chronic immune dysfunction that leaves us vulnerable to chronic Lyme disease and other chronic illnesses is by doing everything you can in your everyday life to strengthen the cells in your body. To do this, providing your cells with proper nourishment is essential. These guidelines can help:
- Strive to eat more vegetables than anything else. Vegetables are packed with a greater concentration of the nutrients your cells need to function properly than any other food source. Vegetables are also loaded with beneficial fiber that promotes normal digestion and the balance of microbes in the gut.
- Eliminate processed food products. This automatically cuts out a load of unnecessary carbohydrates, refined oils, and calories your cells don’t need. It also cuts out gluten, a protein in wheat that many people are sensitive to.
- Eat fresh, whole foods. The fresher your food is and the closer to its natural origins, the higher its potential to nourish your cells. In other words, it’s much better to enjoy an apple or a handful of fresh pecans for a snack than a processed “health” food bar that contains apples and nuts.
4. Bring On Calm.
Finding a state of calm is necessary to engage your natural healing processes — and yet pressuring yourself to relax isn’t exactly conducive to chilling out. It can be a vicious cycle, and breaking free really requires committing to creating a healing environment within the body.
A first, vital step is getting enough sleep. Your cells rely on that time to regenerate, so you need at least eight hours of good quality sleep every night.
If you have trouble drifting off, make a habit of turning down the lights, cutting off the technology, and listening to light, restful music for at least an hour before you turn in for bed. Herbs like cannabidiol or CBD oil, motherwort, passion flower, and bacopa can also help you wind down and invite sleep.
5. Purify Your Environment.
Toxic substances can enter the body in three ways: by mouth, breathing, and absorption through the skin. If you live in a contaminated environment (and the vast majority of us do), your wellness potential will be affected by toxic substances.
That’s why it’s essential that you reduce your exposure to environmental toxins whenever you can. Some of the simplest, most impactful ways to do that: Opt for organic foods when feasible, filter your water and air, and choose non-toxic cleaning supplies and beauty products.
6. Move As Much As You Can.
Staying in motion increases blood flow, which washes out toxins, stimulates healing, and increases oxygen and nutrient delivery to cells. That said, if you have chronic illness and overdo it, there’s a risk of setback and post-exertional malaise (PEM), which is a worsening of symptoms such as fatigue, sleeplessness, cognitive issues, pain, dizziness, and more.
So keep in mind that becoming active again must be a delicate balance between moving enough to gain benefit, but not so much that it aggravates inflamed tissues and causes further damage. Some suggestions for starting slow and easy include going at your own pace, trying restorative exercise like yoga and qigong, swimming slow laps, and stopping before the movement starts to make you feel bad.
Final Thoughts
Natural herbal therapy reduces inflammation and enhances immune function, while at the same time suppressing stealth microbes and protecting our cells. Because herbal therapy is so remarkably safe, it can be continued for a lifetime.
To maximize its effectiveness, combine herbs with eating a clean diet, eliminating unnecessary toxins, managing stress, and exercising regularly. When you take steps to care for your immune system properly and nourish your cells, your path to recovery becomes a little bit brighter.
Dr. Rawls is a physician who overcame Lyme disease through natural herbal therapy. You can learn more about Lyme disease in Dr. Rawls’ new best selling book, Unlocking Lyme.
You can also learn about Dr. Rawls’ personal journey in overcoming Lyme disease and fibromyalgia in his popular blog post, My Chronic Lyme Journey.
REFERENCES:
1. Berghoff, W, Chronic Lyme Disease and Co-infections: Differential Diagnosis, Open Neurol J., 2012, 6, p. 158-178
2. A G Barbour and S F Hayes, Biology of Borrelia Species, Microbiol Rev. Dec. 1986, 50(4) p. 381-400
3. A Steer, J Coburn, and L Glickstein, The Evergence of Lyme Disease, J Clin Invest, April 2004, 113(8), p. 1093-1101
4. S Buhner, Healing Lyme, Natural Healing and Prevention of Lyme Borreliosis and Its Coinfections, Raven Press, Silver City, N.M., 2005
5. S Buhner, Healing Lyme Disease Coinfections, Healing Arts Press, 2013
6. S Buhner, Natural Treatment for Lyme Coinfections, Healing Arts Press, 2015
7. Nicholson G, Chronic Bacterial and Viral Infections in Neurodegenerative and Neurobehavioral Diseases, May 2008, LABMEDICINE, Vol 39 (5), p. 291-299
8. Hvidsten et al, Borrelia burgdorferi sensu-lato-infected Ixodes ricinus collected from vegetation near the Arctic Circle, Tick Borne Dis., July 6, 2015
9. Masuzawa T, Terrestrial distribution of the Lyme borreliosis agent Borrelia burgdorferi sensu lato in East Asia, Jpn J Infect Dis, Dec 2004, 57 (6), p. 229-235
10. K Waites and D Talkington, Mycoplasma pneumoniae and its Role as a Human Pathogen, Oct 2004, Clinical Microbiology Reviews
11. Hakkarainen, Turrunen, Miettinen, Kaitik, and Jannson, Mycoplasmas and Arthritis, Ann Rheu Dis, 1992, Oct 5 (11): p. 1170-1172
12. Baseman, Joel, et.al., Mycoplasmas: Sophisticated, Reemerging, and Burdened by Their Notoriety, CDC, Journal of Infectious Diseases, Vol 3, No.1, Feb 1997
13. Leslie Taylor, ND, Mycoplasmas – Stealth Pathogens (Review article), Jan 2001
14. Razin, Yogev, Naot, Molecular Biology and Pathogenicity of Mycoplasmas, Microbiol Mol Biol Rev, 1998, Dec; 62(4): p. 1094-1156
15. J Rivera-Tapia, N Rodriguez-Preval, Possible role of mycoplasmas in pathogenesis of gastrointestinal diseases, Rev Biomed 2006 17: 132-139
16. www.cdc.gov/ebola/
17. www.cdc.gov/powassan/
18. National Geographic magazine, Nov 2011
19. Diuk-Wasser MA, Vannier E, Krause PJ. Coinfection by Ixodes Tick-Borne Pathogens: Ecological, Epidemiological, and Clinical Consequences. Trends in Parasitology. 2016 Jan; 32(1): 30-42. doi: 10.1016/j.pt.2015.09.008
20. Ebola virus disease. World Health Organization website. https://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease